Table of Contents
-
- Introduction
- Exploring the Benefits of Medicare Coverage for Rehabilitation Services
- Understanding the Different Types of Medicare Coverage for Rehabilitation
- How to Choose the Right Medicare Coverage for Rehabilitation Services
- What to Expect When Seeking Medicare Coverage for Rehabilitation Services
- Navigating the Medicare Coverage Process for Rehabilitation Services
- Conclusion
“Medicare Coverage Rehab: Get the Care You Need, When You Need It!”
Introduction
Medicare Coverage Rehab is a program designed to help individuals who are eligible for Medicare coverage receive the necessary rehabilitation services they need to improve their health and quality of life. This program provides access to physical, occupational, and speech therapy services, as well as other rehabilitative services, to help individuals recover from injury or illness. Medicare Coverage Rehab also covers the cost of durable medical equipment, such as wheelchairs, walkers, and other assistive devices, to help individuals with mobility issues. With the help of Medicare Coverage Rehab, individuals can receive the care they need to improve their health and quality of life.
Find Medicare Plans in 3 Easy Steps
We can help get up to $0 monthly premium Medicare plans
Exploring the Benefits of Medicare Coverage for Rehabilitation Services
Medicare is a federal health insurance program that provides coverage for a variety of medical services, including rehabilitation services. Rehabilitation services are designed to help individuals recover from an illness or injury and improve their overall quality of life. Medicare coverage for rehabilitation services can be a valuable resource for those who need it.
Rehabilitation services covered by Medicare include physical therapy, occupational therapy, speech-language pathology, and other related services. Physical therapy helps individuals regain strength and mobility after an injury or illness. Occupational therapy helps individuals learn how to perform everyday activities, such as dressing, bathing, and cooking. Speech-language pathology helps individuals improve their communication skills.
Medicare coverage for rehabilitation services can be beneficial for those who need it. Medicare covers 80% of the cost of rehabilitation services, which can help reduce the financial burden of medical bills. Additionally, Medicare coverage for rehabilitation services can help individuals access the care they need in a timely manner. Medicare also covers the cost of durable medical equipment, such as wheelchairs and walkers, which can help individuals with mobility issues.
Medicare coverage for rehabilitation services can also help individuals access specialized care. Medicare covers the cost of services provided by certified rehabilitation professionals, such as physical therapists, occupational therapists, and speech-language pathologists. These professionals are trained to provide specialized care that can help individuals recover from an illness or injury and improve their overall quality of life.
In conclusion, Medicare coverage for rehabilitation services can be a valuable resource for those who need it. Medicare covers 80% of the cost of rehabilitation services, which can help reduce the financial burden of medical bills. Additionally, Medicare coverage for rehabilitation services can help individuals access the care they need in a timely manner and access specialized care from certified rehabilitation professionals.
Understanding the Different Types of Medicare Coverage for Rehabilitation
Medicare is a federal health insurance program that provides coverage for a variety of medical services, including rehabilitation. Depending on your individual needs, there are several types of Medicare coverage available for rehabilitation services.
Part A: Part A is the hospital insurance portion of Medicare. It covers inpatient hospital care, skilled nursing facility care, hospice care, and some home health care services. If you are admitted to a hospital or skilled nursing facility for rehabilitation, Part A will cover the cost of your stay.
Part B: Part B is the medical insurance portion of Medicare. It covers doctor visits, outpatient care, medical supplies, and preventive services. Part B also covers some types of rehabilitation services, such as physical therapy, occupational therapy, and speech-language pathology services.
Part C: Part C, also known as Medicare Advantage, is an alternative to Original Medicare. It is offered by private insurance companies and provides the same coverage as Parts A and B, plus additional benefits such as vision, hearing, and dental coverage. Some Medicare Advantage plans also cover additional rehabilitation services, such as chiropractic care and acupuncture.
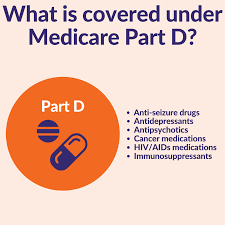
Part D: Part D is the prescription drug coverage portion of Medicare. It covers the cost of prescription drugs, including those used for rehabilitation.
Medicare Supplement Insurance: Medicare Supplement Insurance (also known as Medigap) is a type of private insurance that helps cover the out-of-pocket costs associated with Original Medicare, such as copayments, coinsurance, and deductibles. It does not cover any additional rehabilitation services.
Understanding the different types of Medicare coverage available for rehabilitation services can help you make an informed decision about which plan is best for you. Be sure to review all of your options carefully and speak with a qualified Medicare representative if you have any questions.
How to Choose the Right Medicare Coverage for Rehabilitation Services
Choosing the right Medicare coverage for rehabilitation services can be a daunting task. With so many options available, it is important to understand the different types of coverage and how they can help you access the care you need. This guide will provide an overview of the different types of Medicare coverage available for rehabilitation services and help you make an informed decision about which coverage is best for you.
Medicare Part A covers inpatient hospital care, including rehabilitation services. This coverage includes physical, occupational, and speech therapy services provided in a hospital setting. It also covers the cost of any necessary medical equipment, such as wheelchairs or walkers.
Medicare Part B covers outpatient services, including rehabilitation services. This coverage includes physical, occupational, and speech therapy services provided in an outpatient setting. It also covers the cost of any necessary medical equipment, such as wheelchairs or walkers.
Medicare Part C, also known as Medicare Advantage, is a private health insurance plan that covers all of the services covered by Parts A and B, as well as additional services such as vision and dental care. Some Medicare Advantage plans also cover rehabilitation services.
Medicare Part D covers prescription drugs. This coverage can help you pay for medications that are necessary for your rehabilitation services.
Finally, Medicare Supplement Insurance (Medigap) is a private health insurance plan that helps cover the costs of services not covered by Medicare. Medigap plans can help cover the cost of rehabilitation services, as well as other medical expenses.
When choosing the right Medicare coverage for rehabilitation services, it is important to consider your individual needs and budget. Be sure to research all of your options and speak with a qualified health care professional to determine which coverage is best for you.
Find Medicare Plans in 3 Easy Steps
We can help get up to $0 monthly premium Medicare plans
What to Expect When Seeking Medicare Coverage for Rehabilitation Services
When seeking Medicare coverage for rehabilitation services, it is important to understand what to expect. Medicare is a federal health insurance program that provides coverage for a variety of medical services, including rehabilitation services.
In order to be eligible for Medicare coverage for rehabilitation services, you must meet certain criteria. Generally, you must be 65 years of age or older, or have a qualifying disability. Additionally, you must be enrolled in Medicare Part A and Part B.
Once you have determined that you are eligible for Medicare coverage for rehabilitation services, you will need to select a provider. Medicare-approved providers are those that have been approved by the Centers for Medicare & Medicaid Services (CMS). It is important to note that not all providers are Medicare-approved, so it is important to check with your provider to ensure they are approved.
Once you have selected a Medicare-approved provider, you will need to obtain a referral from your primary care physician. This referral will be used to determine the type of rehabilitation services that are covered by Medicare.
Once you have obtained a referral, you will need to contact your Medicare-approved provider to schedule an appointment. During this appointment, your provider will assess your condition and determine the type of rehabilitation services that are necessary.
Once your provider has determined the type of rehabilitation services that are necessary, they will submit a claim to Medicare for reimbursement. Medicare will then review the claim and determine the amount of coverage that is available.
It is important to note that Medicare coverage for rehabilitation services is limited. Medicare will only cover medically necessary services that are deemed to be reasonable and necessary for the treatment of your condition. Additionally, Medicare will only cover services that are provided by a Medicare-approved provider.
In conclusion, when seeking Medicare coverage for rehabilitation services, it is important to understand the eligibility requirements, select a Medicare-approved provider, obtain a referral from your primary care physician, and understand the limitations of coverage. By following these steps, you can ensure that you receive the coverage you need for your rehabilitation services.
Navigating the Medicare Coverage Process for Rehabilitation Services
Navigating the Medicare coverage process for rehabilitation services can be a daunting task. Understanding the various coverage options and eligibility requirements is essential for ensuring that you receive the care you need. This guide will provide an overview of the Medicare coverage process for rehabilitation services, including eligibility requirements, coverage options, and how to apply.
Eligibility Requirements
In order to be eligible for Medicare coverage for rehabilitation services, you must be enrolled in Medicare Part A and Part B. Additionally, you must meet certain medical criteria, such as having a disability or illness that requires rehabilitation services.
Coverage Options
Medicare covers a variety of rehabilitation services, including physical therapy, occupational therapy, speech-language pathology, and prosthetic and orthotic services. Medicare Part A covers inpatient rehabilitation services, while Medicare Part B covers outpatient rehabilitation services.
How to Apply
To apply for Medicare coverage for rehabilitation services, you must first contact your doctor or healthcare provider to determine if you are eligible for coverage. Once you have been deemed eligible, you can then contact your local Medicare office to apply for coverage.
Navigating the Medicare coverage process for rehabilitation services can be a complex process. However, understanding the eligibility requirements, coverage options, and how to apply can help ensure that you receive the care you need.
Find Medicare Plans in 3 Easy Steps
We can help get up to $0 monthly premium Medicare plans
Conclusion
In conclusion, Medicare coverage for rehab services is an important benefit for those who need it. It can help cover the cost of necessary treatments and therapies, allowing individuals to get the care they need to improve their health and quality of life. While there are some restrictions and limitations to Medicare coverage for rehab services, it is still a valuable resource for those who need it.