Medicare
What is Medicare?
Medicare is a federal health insurance program in the US for specific groups of people. These are:
65+: Most Medicare recipients fall into this category and get automatic coverage when they turn 65.
Under 65 with disabilities: People with qualifying disabilities like long term physical or mental impairments may be eligible for Medicare.
People with End-Stage Renal Disease (ESRD): This includes people with permanent kidney failure who need dialysis or a kidney transplant.
Medicare Structure
Medicare is broken down into different parts, each covering different types of care:
Medicare Part A (Hospital Insurance):
Covers inpatient hospital care, skilled nursing facility care, hospice care and some home health services.
Most people are eligible for premium-free Part A if they or their spouse have worked and paid Medicare taxes for at least 10 years.
Medicare Part B (Medical Insurance):
Covers outpatient services, including doctor visits, preventive services, medical supplies and some home health services.
Beneficiaries pay a monthly premium for Part B which varies based on income.
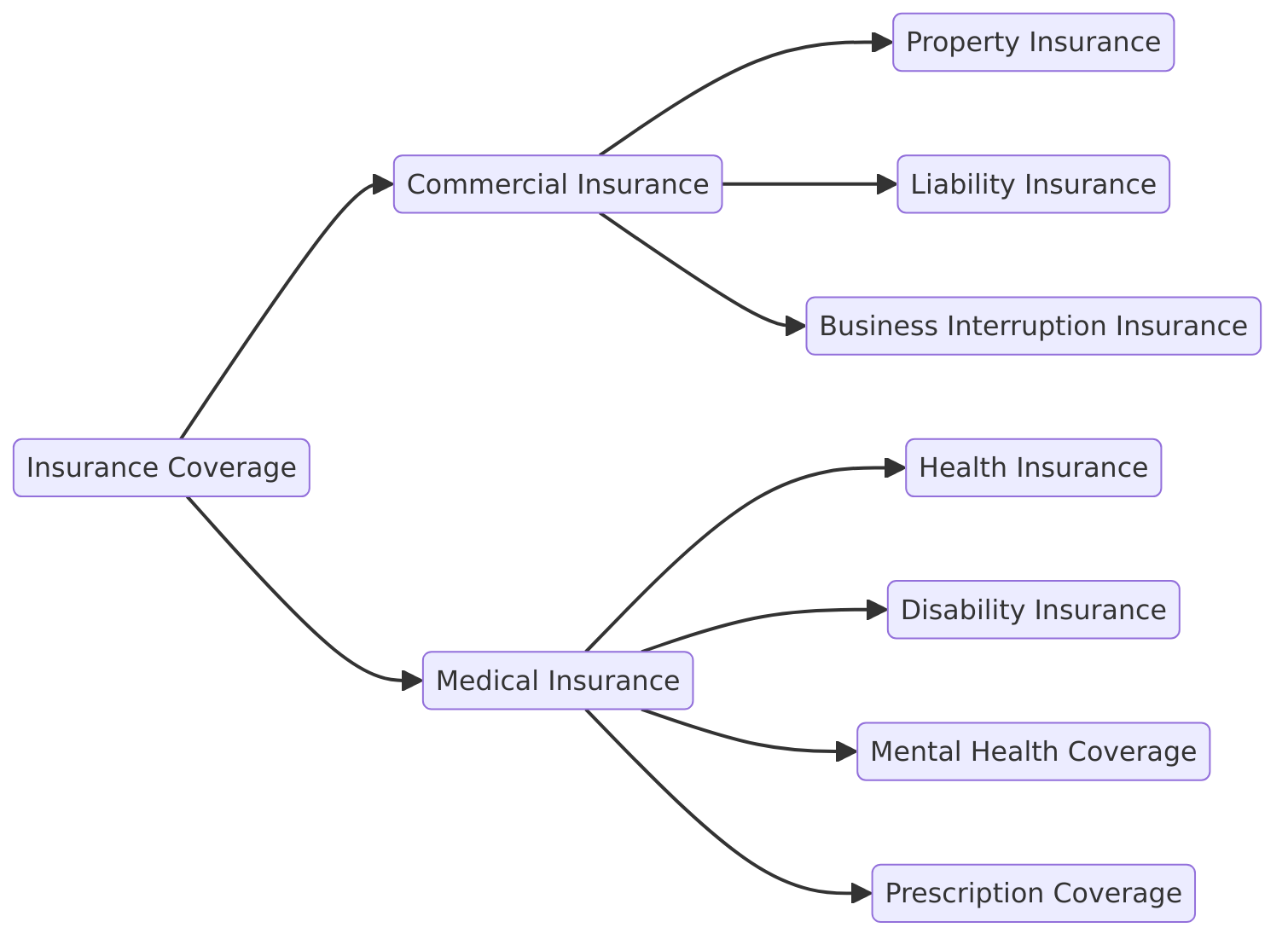
Medicare Part C (Medicare Advantage):
An alternative to Original Medicare offered by private insurance companies approved by Medicare.
Combines the benefits of Part A and Part B and often includes extra services like vision, dental and hearing. Some plans may also cover incontinence supplies.
Medicare Part D (Prescription Drug Coverage):
Covers prescription medications.
Offered through private insurers and beneficiaries must choose and enroll in a plan that fits their needs.
Medicare Features
Universal Coverage: Designed for broad coverage of people, Medicare is a safety net.
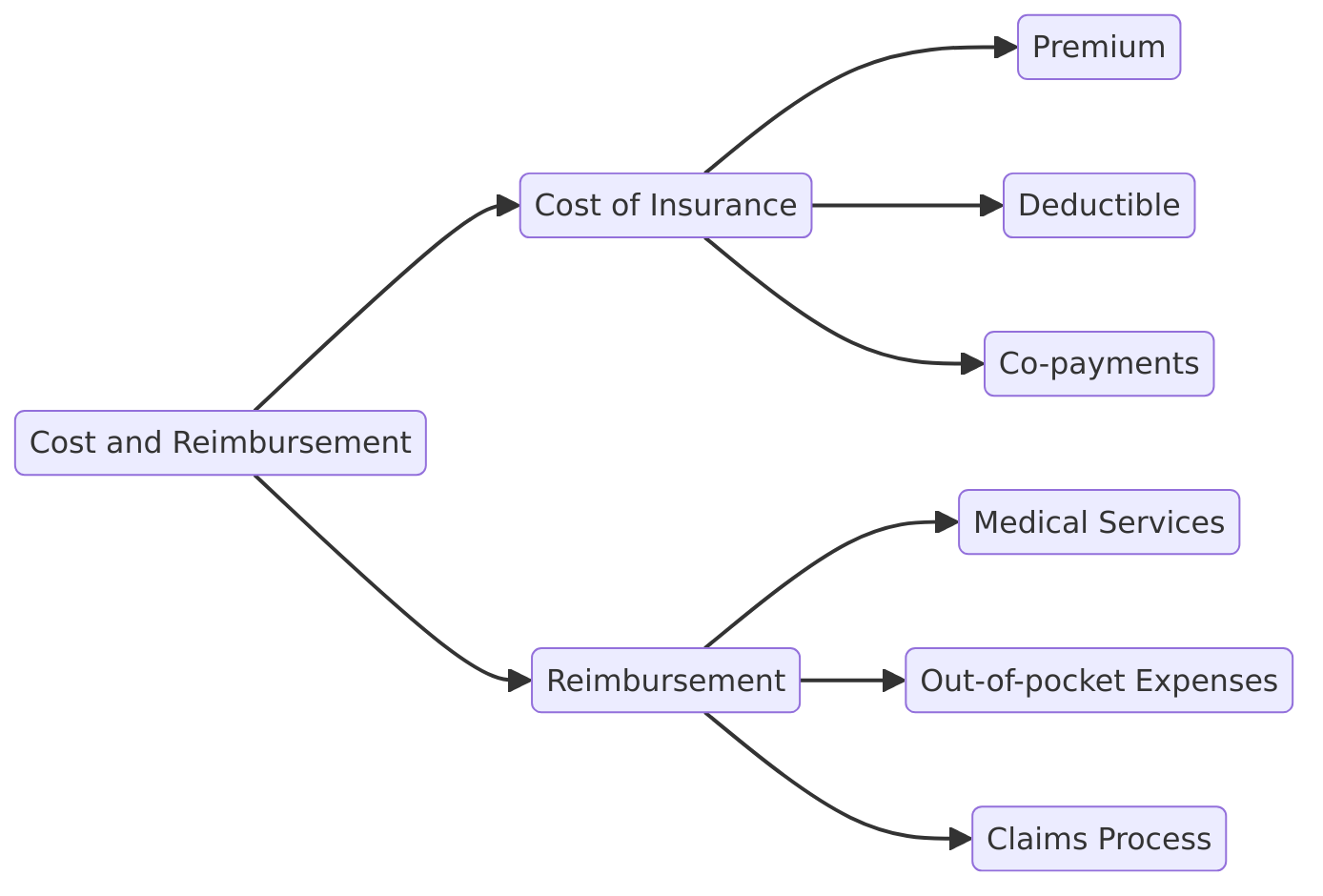
Cost Sharing: Medicare has cost sharing like premiums, deductibles and copays. Medigap can help with those costs.
Coverage: While Medicare is broad, it doesn’t cover everything, like routine dental, vision and hearing services or incontinence supplies like adult diapers or PureWick external catheters (except in certain circumstances). For any item to be covered it must fall under a specific Medicare benefit category and meet medical necessity and applicable Medicare statutory requirements.
Find Medicare Plans in 3 Easy Steps
We can help get up to $0 monthly premium Medicare plans
Medicare is the base layer of coverage but navigating non-standard items like external catheters requires attention to eligibility, documentation and additional benefits through Part C plans.
Medicare Advantage Plans
Medicare Advantage plans are an alternative to Original Medicare with extra benefits and coverage options. These plans are offered by private insurance companies approved by Medicare and must cover everything Original Medicare covers. But Medicare Advantage plans often go beyond the basics and offer extra services like dental, vision and hearing. When it comes to external catheters Medicare Advantage plans have different rules and requirements. Review your plan documentation and contact your insurance provider to see if your Medicare Advantage plan covers external catheters. Be proactive and know your benefits so you can make informed decisions about your care.
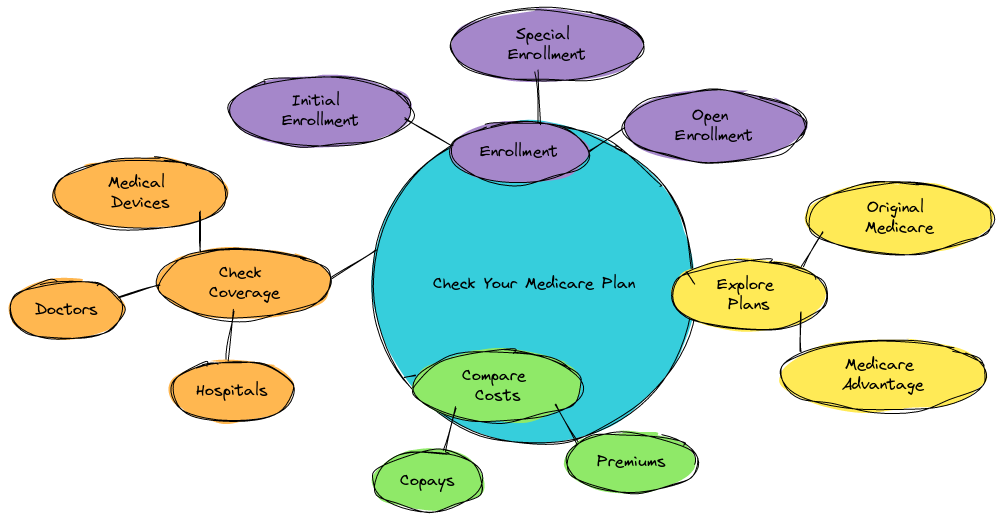
Medicare Enrollment Periods
Knowing Medicare enrollment periods is key especially if you’re thinking of enrolling in a Medicare Advantage plan or switching from Original Medicare to a Medicare Advantage plan. The Medicare Open Enrollment Period is usually from October 15 to December 7 each year when you can make changes to your Medicare coverage. There are also Special Enrollment Periods (SEPs) for certain life events like moving to a new area or losing employer coverage. If you want to enroll in a Medicare Advantage plan that covers external catheters you need to know the enrollment periods and deadlines. Be aware of these timelines so you can take advantage of the best options for you.
Medicare Coverage for Urinary Incontinence
External Catheters and Medicare Coverage
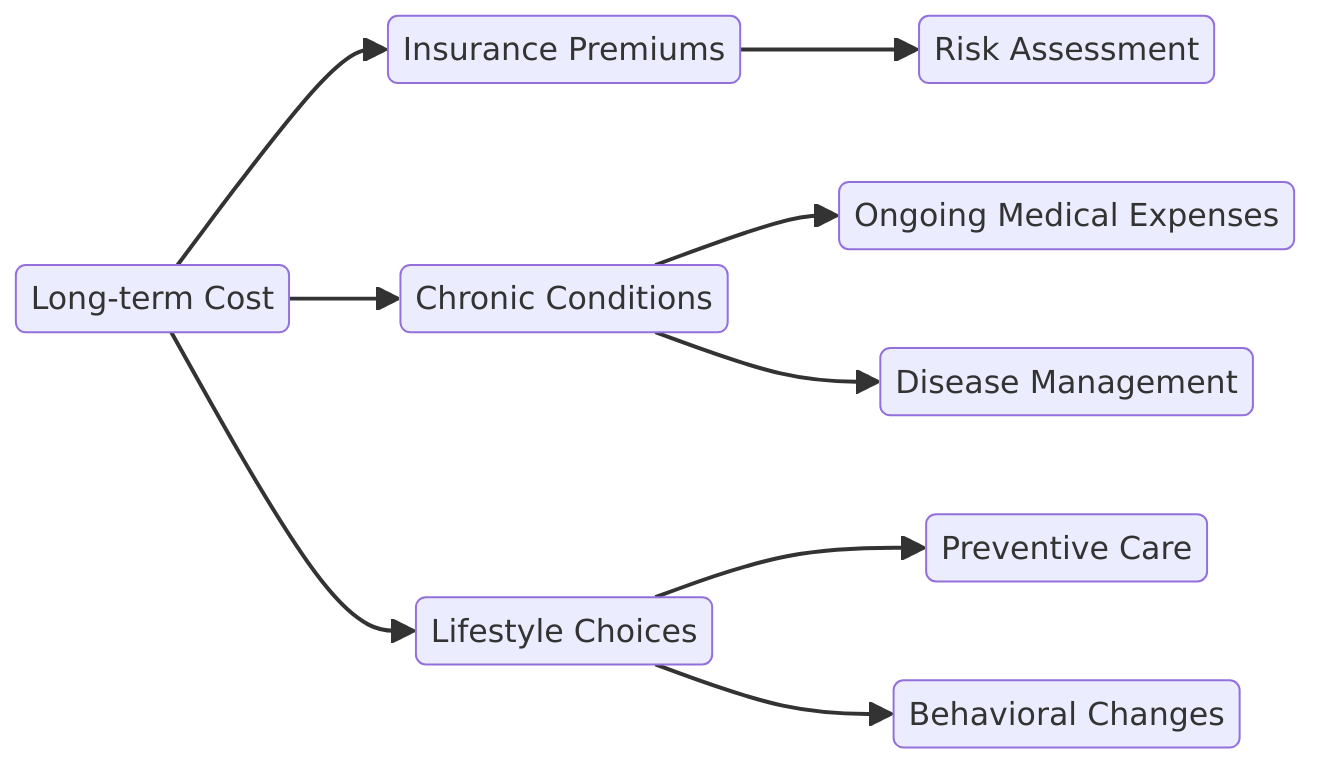
Urinary incontinence affects millions in the U.S., and for many, external catheters covered by Medicare are the solution. Medicare through its Durable Medical Equipment (DME) benefits covers partial coverage for external catheters under certain circumstances.
Coverage Scope: Medicare covers external catheters for urine management especially as a substitute for Foley catheters which are invasive and have higher risk of infection. External catheters are a less invasive option for patients with urinary incontinence.
Medicare Part B:
80% of the cost of external catheters and supplies.
20% out of pocket unless covered by supplemental insurance like Medigap.
Eligibility Requirements:
Covers under the Prosthetic Device benefit (Social Security Act § 1861(s)(8)).
Patient must demonstrate medical necessity through proper documentation including a prescription and evidence of chronic or permanent need for the device.
Billing Codes for External Catheters
Billing codes for external catheters are crucial for accurate reimbursement and coverage under Medicare. The Healthcare Common Procedure Coding System (HCPCS) codes for external catheters are as follows:
A4217: External urinary collection device, male
A4450: External urinary collection device, female
A4452: External urinary collection device, pediatric
A6590: External urinary catheter, monthly supply
A7001: Non-disposable canister for external urinary catheter
A7002: Tubing for external urinary catheter
Using the correct HCPCS code when billing for external catheters is essential to ensure accurate claim payment. The Pricing, Data Analysis, and Coding (PDAC) contractor maintains a variety of resources to assist suppliers in determining the appropriate code for Medicare billing. This ensures that claims are processed correctly and that beneficiaries receive the coverage they are entitled to.
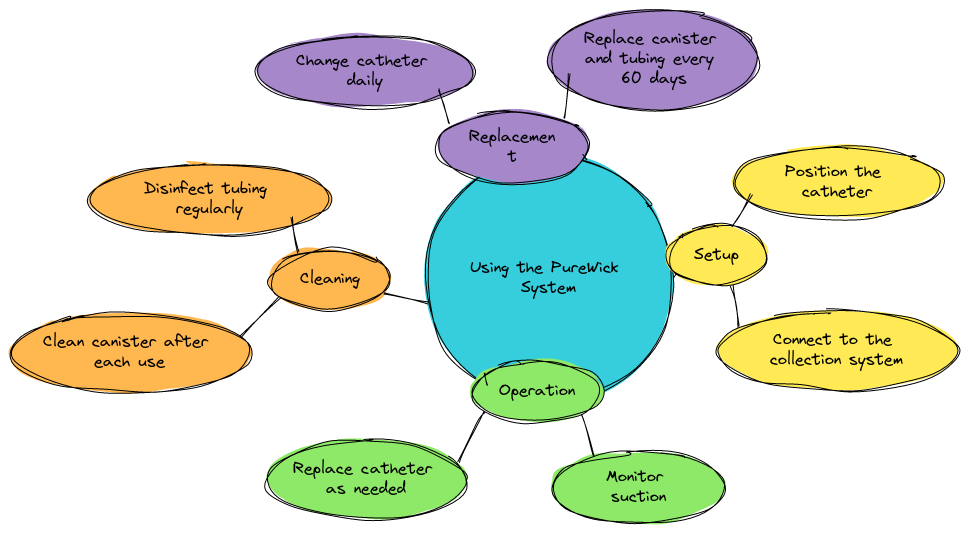
PureWick Urine Collection System
The PureWick® Urine Collection System has changed the face of urinary incontinence management with its non-invasive design. Unlike traditional catheters it uses a soft external wick and a low-pressure suction unit to collect urine, patient comfort and hygiene.
How it Works:
External wick placed between the legs wicks urine away from the body.
Low-pressure suction pump directs urine through tubing into a collection canister.
Medicare and Medicaid Billing:
PureWick System is classified as Durable Medical Equipment (DME).
With proper documentation of medical necessity it can be billed under Medicare Part B and some Medicaid services. Coverage for the PureWick system is subject to Local Coverage Determination (LCD) criteria which outlines the circumstances under which the device can be covered based on medical necessity and inclusion in a defined Medicare benefit category.
Recent Medicare Coverage Update:
March 2024 CMS approved Medicare coverage for the PureWick system under certain circumstances. This means eligible patients can now get this device at a lower cost.
How it Works
The PureWick Urine Collection System is a non-invasive, external catheter system for urinary incontinence management. It consists of a soft external wick that rests against the body and a low-pressure suction unit. The suction unit can be placed on a bedside table or a flat surface near the bed. The PureWick system reduces the risk of complications associated with traditional catheters like UTIs and skin irritation. It provides a comfortable and hygienic solution for patients to manage urinary incontinence.
Find Medicare Plans in 3 Easy Steps
We can help get up to $0 monthly premium Medicare plans
Coverage Details
Documentation: Medicare requires a healthcare provider to document medical necessity for the PureWick system or any external catheter.
Billing Codes: Proper coding like HCPCS codes A4327 and A4328 for female external urinary collection devices.
Patient Responsibility: Medicare covers 80% of approved cost, 20% patient responsibility unless supplemental insurance applies.
External catheters and the PureWick system being covered by Medicare is a big step forward in addressing urinary incontinence, offering patients non-invasive and comfortable solutions and some financial relief. For personalized help with Medicare coverage for urinary incontinence devices call Medicare Advisors Insurance Group LLC.
Medicare Part B and PureWick
Medicare Part B covers Durable Medical Equipment (DME) including external catheters like the PureWick system. However Medicare Part B coverage for PureWick has certain requirements and limitations. To be eligible for Medicare Part B coverage the PureWick system must be ordered by a healthcare provider and meet medical necessity. Also the system must be purchased from a Medicare approved supplier. Be sure to review your Medicare Part B coverage and consult with your healthcare provider to see if the PureWick system is covered under your plan so you can get the equipment you need and minimize out of pocket expense.
DMEPOS and Medicare
What is DMEPOS?
DMEPOS stands for Durable Medical Equipment, Prosthetics, Orthotics, and Supplies. This includes a broad range of medical devices and supplies used to treat many medical conditions. These items are used in the home and help patients live independently.
Examples of DMEPOS:
DME: Wheelchairs, walkers, hospital beds, oxygen equipment etc.
Prosthetics: Devices that replace a missing body part, like artificial limbs.
Orthotics: Braces or supports for weak or ineffective joints or muscles.
Supplies: Disposable items used to operate or complement DME, like external catheters, tubing and ostomy bags.
Relevance to Urinary Incontinence:
External catheters like the PureWick Urine Collection System fall under DMEPOS when used to manage urinary incontinence.
DMEPOS Coverage Criteria
To be eligible for Medicare coverage DMEPOS items must meet strict eligibility and usage requirements.
Medical Purpose:
The item must be used primarily for a medical purpose and not for convenience or comfort.
Durable:
Items must be durable and reusable, used multiple times over a period of time.
Prescribed by a Healthcare Provider:
A doctor’s order is required with medical necessity of the equipment or supplies.
Medicare Statute and Regulation:
The item must meet all Medicare guidelines, including those in the Social Security Act. Also must meet all Medicare statute and regulation, including medical necessity and billing rules.
DMEPOS and External Catheters
External catheters like those used with the PureWick system are DMEPOS because they meet:
Primary Medical Use: Used to manage urinary incontinence.
Durable: While individual components like tubing are reusable, external catheters are single use items that complement durable equipment like suction pumps.
Medical Necessity: Medicare requires documentation to support the patient’s need for external catheters:
Diagnosis of chronic urinary incontinence. Patients with permanent urinary incontinence may be eligible for Medicare coverage for necessary supplies and devices to manage incontinence.
A statement of medical necessity.
Male external catheter: Medicare requires documentation to support the patient’s need for male external catheters, including a diagnosis of chronic urinary incontinence and a statement of medical necessity.
Patient Costs under Medicare
Medicare Part B covers 80% of approved DMEPOS items after the patient meets their annual deductible.
The remaining 20% is out of pocket unless the patient has supplemental insurance like Medigap.
Why DMEPOS Criteria Matter
Understanding DMEPOS criteria is important for patients and caregivers to get reimbursement for medical equipment. For devices like the PureWick Urine Collection System meeting these criteria can help reduce the financial burden on families with urinary incontinence.
Need help with DMEPOS and documentation? Contact Medicare Advisors Insurance Group LLC. We’ll make it easy for you and advocate for your healthcare.
Check Your Medicare Plan
How to Check Your Plan
To get coverage for the PureWick Urine Collection System or any other medical equipment you need to review your Medicare plan and benefits. Here’s how:
Contact Your Medicare Advantage Provider:
Call your Medicare Advantage (Part C) plan.
Tell them about the PureWick system and ask if it’s covered.
Ask about cost sharing, copays, deductibles or coinsurance.
Review Your Plan Documents:
Read coverage booklets, plan summaries or online portals for DME and urological supplies.
Look for HCPCS codes A4327 (external female urinary collection devices) or A7002 (tubing and accessories).
Talk to Your Healthcare Provider:
Discuss your condition with your doctor to see if the PureWick system is medically necessary.
Get a prescription and supporting documentation to support your claim.
Coverage Options
Medicare plans and other insurance carriers offer different levels of coverage for the PureWick system. Here’s a breakdown:
Medicare Advantage Plans:
Extra Benefits: Original Medicare doesn’t cover the PureWick system but many Medicare Advantage plans do. Additional benefits.
Plan Specific Coverage: Coverage varies by carrier so use the Medicare Plan Finder or contact your carrier for details.
Medicaid Services:
State Coverage: Medicaid is state run and coverage for the PureWick system may vary.
Eligibility: Contact your state’s Medicaid office to find out about coverage and eligibility requirements.
Private Insurance Plans:
Varying Coverage: Some private carriers may cover the PureWick system fully or partially depending on the plan.
What to Ask:
Does my plan cover the PureWick system or similar external catheters?
Is prior authorization required or proof of medical necessity?
What’s the out of pocket cost?
Plan Tips
Verify Benefits Annually:
Plan benefits change every year so make sure coverage for the PureWick system is still in place during open enrollment.
Supplemental Options:
If your plan doesn’t cover the PureWick system consider purchasing Medigap or supplemental insurance to offset out of pocket costs.
For personalized guidance contact Medicare Advisors Insurance Group LLC. We can help you evaluate your options, compare plans and maximize your benefits.
Medicare Myths
There are several myths about Medicare coverage especially when it comes to external catheters. One myth is that Medicare only covers internal catheters not external catheters. But Medicare Part B covers external catheters including the PureWick system as long as medically necessary. Another myth is that Medicare Advantage plans don’t cover external catheters. But many Medicare Advantage plans do cover external catheters including the PureWick system. It’s important to review your Medicare coverage and talk to your healthcare provider to see what options are available to you. By debunking these myths you can make better informed decisions about your healthcare and coverage.
PureWick Coverage through Medicare
ProMed DME and the PureWick System
For patients who need help managing the cost of the PureWick Urine Collection System when Medicare coverage is not available or limited, ProMed DME is here to help.
Discount Programs:
ProMed DME offers discounts for first time buyers and repeat customers.
New customers can save up to 10% on Starter Sets with Battery to make the initial purchase more affordable.
AutoShip Program:
Enroll in the AutoShip Program for regular discounted deliveries of PureWick supplies.
Benefits:
Door to door delivery.
Knowing you will always have the supplies you need.
Free Shipping:
ProMed DME offers free shipping on all PureWick products so no additional delivery fees.
Insurance Coordination Services:
ProMed DME doesn’t submit claims for PureWick products but can help with:
Gathering the necessary documentation.
Navigating the private insurance reimbursement process.
What to do Next to Manage PureWick Costs
Check Medicaid Benefits:
Contact your state’s Medicaid office to see if they cover external catheters including PureWick.
Medicaid coverage varies by state so eligibility and benefits depend on location and income.
Consider Alternatives:
Talk to your healthcare provider about other Medicare covered options like:
QiVi MEC or FEC external catheters.
Traditional incontinence supplies that may be eligible for Medicare reimbursement.
Other external urinary devices covered under specific HCPCS codes.
Manage Out of Pocket Costs:
Try these to reduce financial burden:
Bulk Purchases: Save per unit by buying in bulk.
Cash Sales Discounts: Take advantage of discounts for paying upfront.
Health Savings Accounts (HSA)/Flexible Spending Accounts (FSA): Use pre-tax dollars to pay for medical supplies like PureWick.
Manufacturer Promotions: Look for seasonal discounts or special offers from PureWick and its retailers.
Contact ProMed DME:
Talk to ProMed DME to see how you can get the PureWick system for an affordable price. They can help you navigate the reimbursement process or find financial assistance options.
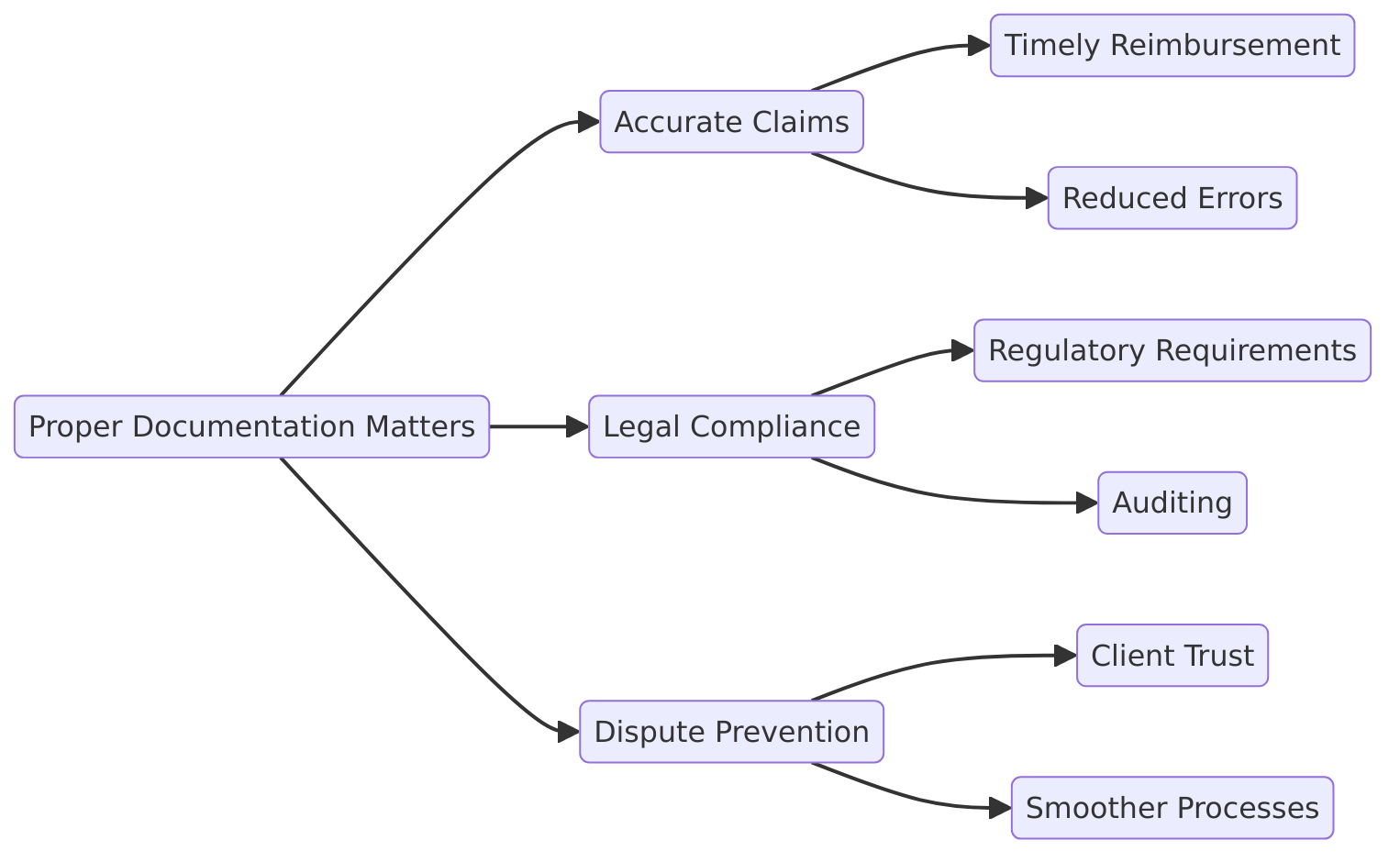
Tips to Get PureWick Covered
Document first
Make sure all prescriptions and medical necessity notes are complete and accurate as these are required for reimbursement.
Research and Compare:
Use the Medicare Plan Finder to find plans that offer additional benefits such as external catheter coverage.
Talk to a Medicare Advisor:
Contact Medicare Advisors Insurance Group LLC for personalized help with Medicare, Medicaid and private insurance for PureWick or similar products.
By using the resources available and managing costs, patients can get the benefits of the PureWick system with less financial burden. For advice and solutions contact Medicare Advisors Insurance Group LLC.
More Information
Contact Medicare
Getting Medicare coverage for medical devices like the PureWick® Urine Collection System can be confusing. Getting detailed and personalized information is key to making an informed decision. Here’s how you can get the answers you need from Medicare:
Medicare Helpline:
Call 1-800-MEDICARE (1-800-633-4227) for 24/7 help.
TTY users call 1-877-486-2048.
Talk to a Medicare representative to:
Find out if the PureWick system or other external catheters are covered under your plan. Using external catheters can reduce clinical complications like urinary tract infections (CAUTI) and incontinence-associated dermatitis (IAD) and lead to shorter hospital stays and better patient outcomes.
Get information on eligibility and documentation.
Medicare.gov:
Visit the official Medicare.gov website for more information including:- DME and incontinence supply coverage guidelines.
Medicare Plan Finder tool to compare Medicare Advantage plans that offer additional benefits for urinary incontinence devices.
State Health Insurance Assistance Program (SHIP):
Contact your local SHIP counselor for free Medicare help.
They can help you understand your benefits, compare plans and find additional coverage.
Medicare Policy Articles and Guidance
Medicare policy articles and guidance provide essential information for healthcare providers, suppliers, and beneficiaries on Medicare coverage and reimbursement for external catheters. The Centers for Medicare and Medicaid Services (CMS) publishes policy articles and guidance on various topics, including durable medical equipment, prosthetics, orthotics, and supplies (DMEPOS).
Some relevant Medicare policy articles and guidance for external catheters include:
Medicare Coverage of External Urinary Catheters (CMS Publication 100-03, Medicare National Coverage Determinations Manual, Chapter 1, Section 180.2)
Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) (CMS Publication 100-04, Medicare Claims Processing Manual, Chapter 20)
Local Coverage Determination (LCD) for Urological Supplies (L33803)
These policy articles and guidance provide information on Medicare coverage, billing, and reimbursement for external catheters, as well as requirements for medical necessity, documentation, and supplier standards. Healthcare providers and suppliers should consult these resources to ensure compliance with Medicare regulations and to provide accurate information to beneficiaries. This helps in managing urinary incontinence effectively while reducing clinical complications and ensuring that patients receive the necessary support and equipment.
Be Informed to Manage Urinary Incontinence
By using Medicare’s resources and working with healthcare providers, patients can navigate the Medicare maze with confidence. Follow these steps to make the best decision for your health and wallet:
Stay Current:
Coverage changes over time. Review your plan during Open Enrollment each year to make sure it’s still right for you.
Talk to Experts:
Talk to healthcare providers and Medicare advisors for personalized advice on coverage and alternatives.
Use More Tools:
Use the Medicare Plan Finder to find plans that cover PureWick.
Private insurance, Medicaid or financial assistance programs if there’s a gap in coverage.
Contact Medicare Advisors Insurance Group LLC for personalized help with Medicare or to find cost saving options for PureWick. We can make it easy for you and get you the care and equipment you need.
frequently asked questions
Is PureWick covered by Medicare or Medicaid?
Medicare and Medicaid coverage for PureWick systems varies. While Medicare does not typically cover PureWick external female catheters as standard durable medical equipment (DME), Medicaid coverage depends on state policies and medical necessity.
How do you get Medicare to pay for PureWick?
Currently, there is no way to get Medicare to pay for PureWick systems, as they are not classified under covered durable medical equipment. Advocating for coverage or exploring private insurance options might be alternatives.
Why did Medicare stop paying for PureWick?
Medicare has not officially covered PureWick systems, so the question of stopping coverage does not apply. The system does not meet the DME coverage requirements under Medicare.
Does Medicare cover an external female catheter?
No, Medicare does not cover external female catheters like the PureWick system. It only covers internal catheters when medically necessary.
What is the cost of PureWick?
The cost of a PureWick system can range from $300 to $600, with additional expenses for ongoing supplies such as catheters. Pricing may vary depending on the vendor.